Spinal infection is a rare but often severe form of the disease that occurs when bacteria, fungi, or viruses invade the spinal tissues. Spinal infections may arise spontaneously or as a secondary condition, such as after a spine surgery.
The symptoms of a spinal infection tend to develop very slowly. Spinal infections take between 3 days and 3 months to notice.
Common warning signs of a spinal infection include
- Pain that is worse with movement and doesn’t respond to rest and medication
- Neck stiffness
- Fever
- Chills
- Swelling or redness at the infection site
- Night pain
- Unexplained weight loss
- Bowel and bladder incontinence
- Progressive development of severe back pain with limited mobility
- Weakness, numbness or tingling in the arms and legs
If you suspect that you have a spinal infection, then seek medical attention ASAP. Although many of these infections can be treated with antibiotics: A spine infection is considered to be an emergency.
Spinal infections can be caused by either a bacterial or a fungal infection in another part of the body that has been carried into the spine through the bloodstream. The most common source of spinal infections is a bacterium called Staphylococcus Aureus, followed by Escherichia coli.
- Spinal Infections can be diagnosed through a combination of imaging studies and lab work.
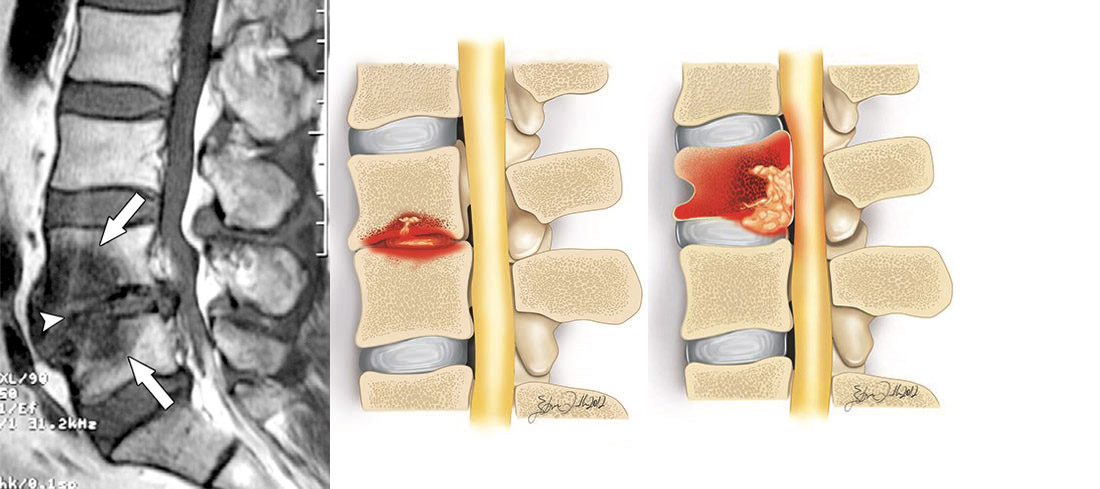
- If you are still in the early stages of an infection, we will likely begin by taking an X-ray. Although x-rays cannot show soft tissues (like spinal discs), they can reveal bone deterioration and loss of disc height.
- To obtain information about both soft tissues and bone health, your doctor may upgrade your exam to an MRI.
- Lab work to diagnose a spinal infection may include examining white blood cell count or markers for inflammation. Specifically, these markers are known as the Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP). These indicators will be unusually high in 85% of all spinal infection cases. In addition, your doctor may also use a Blood Culture to try to isolate the specific pathogen causing your pain.
- Spinal Infections often require long-term Intravenous Antibiotic or Antifungal Therapy and can equate to extended hospitalization time for the patient.
- Immobilization and Bracing may be recommended when there is significant pain or the potential for spine instability.
- Patients generally undergo Antimicrobial therapy for a minimum of six to eight weeks.
Nonsurgical treatment should be considered first when patients have minimal or no neurological deficits and the morbidity and mortality rate of surgical intervention is high.
However, surgery may be indicated when any of the following situations are present:
- Significant bone destruction causing Spinal Instability
- Neurological Deficits
- Sepsis with clinical toxicity caused by an Abscess unresponsive to antibiotics
- Failure Of Needle Biopsy to obtain needed cultures
- Failure Of Intravenous Antibiotics alone to eradicate the infection
The primary goals of surgery are to:
- Debride (clean and remove) the infected tissue
- Enable the infected tissue to receive adequate blood flow to help promote healing
- Restore spinal stability with the use of instrumentation to fuse the unstable spine
- Restore function or limit the degree of neurological impairment
Laminectomy – If your spinal infection is abcessed then we may need to perform a laminectomy (removing the back portion of your vertebra) to relieve pressure on your spinal cord.
Interbody Fusion surgery – We will remove the source of infection from the spine and perform a fusion. Entering the spine from the front or back, we will insert a bone graft that will permanently fuse the two vertebrae together for support.
Vertebral Augmentation Procedure – If your vertebra is fractured due to infection then we perform a kyphoplasty or vertebroplasty. We remove the source of infection and inject a medical grade cement into the collapsed vertebra to stabilise it.